
- The Acute Hospital Care at Home waiver program has been extended through Sept. 30, 2030, allowing hospitals to continue delivering inpatient-level services in patients' homes.
- Telehealth coverage will be retroactively applied to any virtual appointments that occurred during the shutdown period, ensuring families aren't left with unexpected bills.
- Policymakers are expected to pursue stand-alone telehealth legislation, potentially reducing future disruptions tied to government funding deadlines.
- Policymakers are expected to pursue stand-alone telehealth legislation, potentially reducing future disruptions tied to government funding deadlines.
After four days of a partial government shutdown, the House passed the $1.2 trillion government funding bill by a 217-214 vote on Feb. 3, 2026. The resolution of the shutdown is great news for Medicare beneficiaries. Because it means some COVID-era coverage will still be available for things like telehealth visits and acute hospital care-at-home. These programs can make it easier for patients to get the care they need when and where they need it.
Telehealth visits are covered by Medicare
The good news is, Medicare will continue covering telehealth visits for its beneficiaries through Dec. 31, 2027, a significant extension that provides much greater stability for virtual care delivery. This extended timeline gives families and healthcare providers more certainty when planning care.
While the loss of covered telehealth appointments can be an inconvenience to most Americans, its impact is dire for homebound Medicare beneficiaries and their family caregivers. Telehealth appointments save the person we care for the ordeal and discomfort of travel. And they save us time we likely should be spending at work and money spent on gas and parking instead of groceries.
If we live in a rural area, telehealth appointments often mean the difference between accessing care and going without.
Also, in order to receive covered home health care through Medicare, a patient has to have a face-to-face doctor appointment (either in-person or via telehealth) so the doctor can prepare a detailed home health referral order. Here at RubyWell, we help determine eligibility for the Medicare home health benefit and guide families through the referral order process. During the shutdown, our team found that some families simply couldn’t pull off the in-person doctor appointment. So they had to put their plans for accessing home health services on hold.
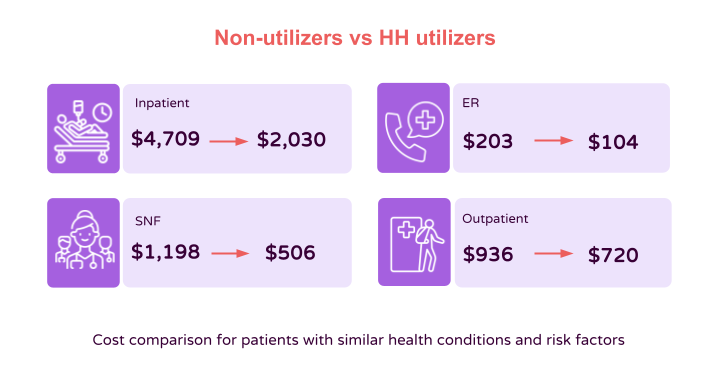
Home health care has shown to improve patient outcomes and lower overall healthcare costs. For instance, patients who receive home health care are admitted to the hospital half as often as patients with similar health conditions who don’t receive home health care. And when we look at the overall healthcare costs of patients with similar health conditions and risk factors, those who receive home health care save Medicare between $2,700 and $3,300 per member per month compared to those who don’t receive home health care. So there were significant down-stream effects to this interruption in telehealth coverage.
Telehealth visit coverage has also resumed for hospice patients’ required face-to-face encounters prior to their third or subsequent benefit period.
Acute care hospital at home is covered by Medicare
The Acute Care Hospital at Home program, which was also halted during the shutdown, has now been extended through Sept. 30, 2030. During the shutdown period, some hospital at home patients had to return to hospitals to receive care. That meant higher health care costs, more exposure to germs and disease, and more time and money spent by family caregivers who had to travel back and forth to a hospital to visit a loved one.
Thankfully, hospitals can now continue to deliver inpatient-level services in a patient's home for another 4+ years. So patients get to receive the care they need in the comfort and safety of home (not to mention good home cooking). And family caregivers can spend less time on the road.
Looking Ahead
Lawmakers from both parties have expressed support for telehealth, with attention now shifting toward stand-alone legislation rather than extensions tied to short-term funding measures. This shift could provide even greater long-term stability for families relying on virtual care. RubyWell will continue to monitor updates to Medicare rules and coverage, sharing any new information with family caregivers as it becomes available.
If you found the information here helpful, please share this article with other family caregivers you may know.









