
- 12 million Medicare beneficiaries may be eligible for covered home health care, but many don’t receive it.
- To qualify for the Medicare home health benefit, a Medicare beneficiary needs to be homebound, require intermittent skilled care, and be under the care of a doctor who will provide a home health referral order.
- For those on Original Medicare, RubyWell can predict eligibility for the Medicare home health benefit, and guide families through the process of discussing the value of a home health referral order with their doctor.
- Covered home health services must be medically necessary and do not include 24-hour care, meal delivery, homemaker services, or personal care not tied to medical needs.
If someone we love is aging at home and has a health condition that makes it hard for them to leave home without assistance, we might be wondering if Medicare can cover in-home care costs. Some people know that many state Medicaid programs cover this. But the person requiring care has to meet strict income and asset limits to qualify for Medicaid. That excludes millions of older adults who are covered by Medicare, many of whom still can’t afford to pay out of pocket for care delivered at home.
A lot of family caregivers may also have experience with home health services being ordered for the person we care for, after they’ve been discharged from a hospital or skilled nursing facility. This is often referred to as post-acute home health care, and is covered by Medicare Part A for up to 100 days, as long as the patient continues to meet Medicare's home health eligibility requirements.
But here’s what a lot of families don’t know: Millions of Medicare beneficiaries who live at home with certain chronic health conditions may also be eligible for covered home health care. And this coverage may continue for as long as the care maintains or slows the decline of their health.
RubyWellTM is passionate about helping families understand—then access—the resources we need to keep our loved ones healthy and safe at home. We’ve also done research to prove that, contrary to thinking that it may cost Medicare more money to provide this care, home health services in fact could SAVE Medicare billions of dollars a year.
In this guide, I’ll share what it takes to qualify for Medicare’s home health benefit, and how RubyWell can predict eligibility and guide families through every step of the process to access care.
Understanding Medicare’s home health benefit
Medicare’s home health care benefit is a lifeline for aging adults who need skilled care at home. Unlike long-term custodial care (also referred to as home care), Medicare focuses on medically necessary services like skilled nursing, physical therapy (PT), occupational therapy (OT), or speech therapy (ST). Importantly, a hospital stay is not required to qualify—our loved one can live in the community and still qualify for this care, as long as they meet certain criteria.
How to qualify for home health services under Medicare
To access home health services under Original Medicare, here’s what families need to know:
- Medicare enrollment: The person must be a current Medicare beneficiary through Original Medicare Part A (and ideally Part B, but not necessarily). Those on Medicare Advantage plans (Plan C) can also receive covered home health services, but they may need prior authorization from their Medicare Advantage plan, and may need to pay a co-pay.
- Homebound status: Leaving home must be a major effort because of illness or injury. “Homebound” doesn’t mean bedridden—it means leaving home is difficult and requires assistance from another person or a device like a walker, wheelchair, cane, crutches, or special transportation. Or, the person’s doctor has advised them against leaving home as it could worsen their condition.
- Skilled care: The patient must need part-time or intermittent skilled nursing, PT, OT, or ST (OT alone isn’t enough to start care). Home health care can also be provided by a certified home health aide working under the supervision of a skilled nurse.
- Care by a doctor or allowed provider: The person must be under the care of a doctor, nurse practitioner, clinical nurse specialist, or physician assistant, with a care plan established and reviewed regularly.
- Referral order: The allowed provider must order home health care services after completing a face-to-face visit to assess the patient’s needs and certify eligibility.
- Medicare-certified agency: Home health services must be delivered by a Medicare-certified home health agency.
How to get a home health referral order
Getting started with Medicare home health often feels overwhelming—especially when we’re already busy caring for a loved one at home. It’s not like we can just pick up the phone and call a home health agency and order up care. There are very clear steps that have to be followed. They look something like this:
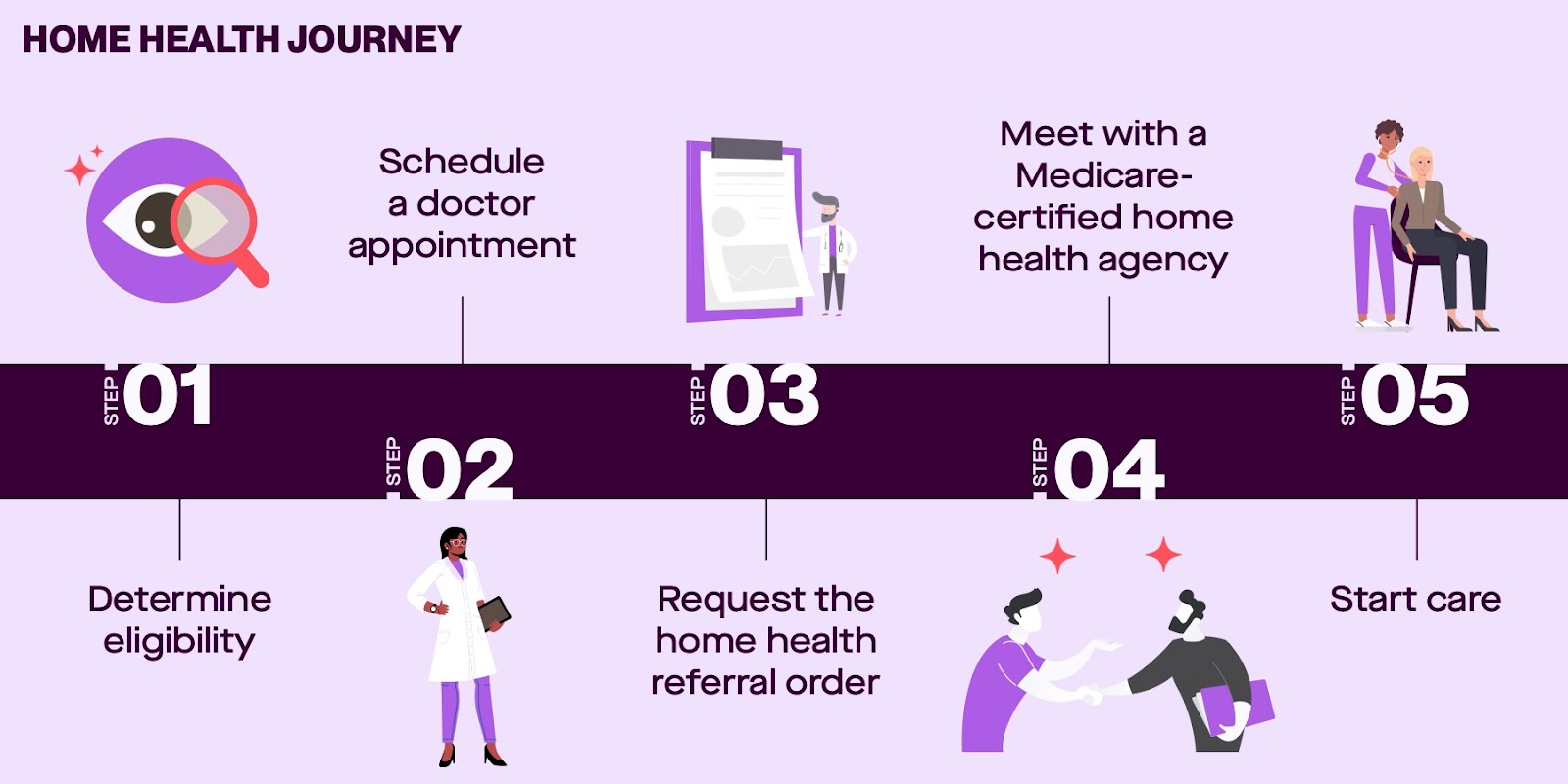
1. Determine eligibility
Because Medicare looks for a combination of health conditions, healthcare events, hospitalization risk factors, and functional limitations to determine home health eligibility, it can be hard to guess if the person we care for may qualify for this benefit. So the first challenge RubyWell set out to solve was how to identify eligible patients in the community who were eligible for covered health services, but not receiving them.
RubyWell's Eligibility Engine can now predict whether someone may qualify for the home health benefit, even before speaking with their doctor. It analyzes mobility, diagnoses, recent health changes, and functional abilities that the care recipient or the caregiver shares with RubyWell. Based on that information and insurance verification, it lets families know if now is the right time to schedule a face-to-face visit with the doctor to discuss home health.
Getting a homebound patient to a doctor’s office can be a major production. So RubyWell only recommends the following steps to patients that the Eligibility Engine predicts may be eligible for covered home health.
2. Schedule a doctor appointment
Let’s say RubyWell finds that my dad is a good fit for home health. They give us the good news and advise us to schedule an in-person doctor appointment with Dad’s primary care doctor. When we make the appointment, it’s important to say that the purpose is to discuss a specific health complaint that’s related to the need for home health care.
Because it can take some time to get on a doctor’s calendar, it’s best to schedule this appointment the same day we learn from RubyWell that the person we care for is likely eligible. Once I know covered care is a possibility for my dad, I’d like it to start as soon as possible!
3. Request the home health referral order
This step sounds easier than it sometimes is. What RubyWell has learned is that some doctors aren’t aware that they can prescribe home health for a patient who’s already living at home under the care of a family member. They, too, think of home health as something that’s ordered after a patient is discharged from a hospital or skilled nursing facility. Also, some doctors may not be familiar with the process of writing a compliant home health order. It’s a detailed document that requires a lot of information in support of the medical necessity for home health.
So RubyWell doesn’t send Dad and me to his doctor empty-handed. They create a personalized Home Health Discussion Guide that captures all the information that Dad’s doctor needs to determine whether home health care is appropriate for him.
It gives details of his health conditions, recent healthcare events, medication list, and functional limitations. It even includes guidance for the doctor for how to prepare a complete and compliant home health order—one that the home health agency is more likely to accept on the first submission, without time-sucking back-and-forths.
Dad and I can share the information in this guide with the doctor during Dad’s in-person visit and use it as the basis of a guided conversation to discuss care options. It’s almost like having a health advocate in the exam room with us.
If Dad’s doctor determines that home health care makes sense for him, they then need to write the Home Health Referral Order and develop a care plan. The care plan outlines all of the home health services that the doctor believes will help Dad live safely at home and lower his risk of hospitalizations. Once the referral order and care plan are complete, the doctor submits them to the Medicare-certified home health agency that RubyWell has assigned to us, via the fax number on the Discussion Guide. Medicare only covers home health services provided by Medicare-certified home health agencies.
4. Meet with a Medicare-certified home health agency
Once the provider has submitted a home health order, the home health agency has 48 hours to review it, ask the prescribing doctor for any missing information if necessary, and accept or deny the patient.
An agency may deny a patient if they don’t have capacity due to staffing limits, coverage area restrictions, specialized service requirements it can’t fulfill or if the patient’s needs are beyond what home health can offer and require acute care. The agency is required to clearly communicate a denial to the patient, including the reason for the denial. And they must explain the appeal process to the patient.
An agency may not deny service to a patient based on the patient’s chronic condition, the family’s availability to provide care, or the potential for the patient’s lack of improvement.
Because RubyWell’s Home Health Discussion Guide provides doctors with detailed information needed to write a compliant home health order, the referral process tends to move smoothly and quickly. This allows care to start sooner with the medically-necessary services provided and covered.
5. Start care
The home health agency that accepts Dad as a patient will schedule an in-home assessment to get to know Dad, his care needs, me, and his living environment. It’s important to note here that an agency may deny service to a patient at this point if they believe they can’t safely serve them due to the physical environment or safety hazards at the home.
If the agency accepts Dad as a patient, they develop a care plan based on the doctor’s guidance on the referral order. It will lay out the home health services he’ll receive and how often he’ll receive them. Then they’ll assign the appropriate care professional(s) and set the visit schedule. Care starts on the day the first care professional arrives to provide the required services.
What home health services are covered by Medicare
Medicare covers the following home health services, provided the patient meets all eligibility criteria:
- Skilled nursing care (part-time or intermittent)
- Physical therapy
- Speech-language pathology
- Continued occupational therapy (if it’s not the sole skilled need)
- Medical social services
- Part-time home health aide services (personal care while skilled needs are present)
Medicare does not cover 24-hour care, meal delivery, homemaker services, or personal care not tied to skilled medical needs. So if the person we care for only needs help with cooking, housekeeping, or errands, these services will not be covered by Medicare.
Common questions about Medicare home health eligibility
Does someone have to be discharged from the hospital to qualify for Medicare home health?
No—a hospital discharge is not required. Older adults who are living in the community can access the benefit if they’re homebound and need skilled home health care.
What does “homebound” mean?
If leaving home takes significant effort, is medically risky, or requires assistance or special equipment, Medicare considers the person homebound. Occasional outings for medical appointments or brief social visits are allowed and don’t disqualify someone from eligibility.
How often can nursing or therapy visits occur?
Medicare covers intermittent or part-time visits. There’s no strict cap on the number or frequency of visits. The maximum number of hours covered per week is 35, however it’s extremely rare for someone to get this much care approved by Medicare. Daily skilled care for an extended period is typically not covered unless it’s medically necessary and appropriate for intermittent care. Visits and frequency are decided by the care plan, which the home health agency reviews regularly.
Can families appeal if care is denied?
Yes. If a Medicare home health agency says services aren’t covered or will end, they must give written notice. Families can appeal, and RubyWell’s technology can re-assess eligibility at that time.
Tips for accessing the Medicare home health care benefit
- Gather as much health information as possible before checking patient eligibility with RubyWell. Track their health issues, mobility challenges, falls, ER or hospital visits, and any decline in their ability to perform daily activities over the past 12 months.
- Advocate for thorough documentation. Make sure healthcare providers note how illness or injury affects the patient’s daily function and independence.
- Be sure that the doctor includes a complete history & physical with any referral for home health.
- If you’re not sure which home health agency to work with, you can ask the doctor for a list of local, Medicare-certified home health agencies. Families working with RubyWell don’t need to worry about this step, as RubyWell refers the patient to a partner home health agency that serves their area.
- If coverage is denied or ends earlier than expected, don’t hesitate to request an appeal.
Why RubyWell makes accessing home health easier
Figuring out when—and how—to request home health support for an aging family member or friend is hard. RubyWell walks us through what to expect at every stage, reducing guesswork and stress. And their Home Health Discussion Guide gives families the information we need to talk knowledgeably with a loved one’s doctor about accessing home health care. It also streamlines the home health referral order process for doctors by gathering all relevant information in one document.
RubyWell helps families avoid missed opportunities for care and gives us the confidence and clarity needed to navigate Medicare’s rules regarding home health services.
Whether the person we care for needs skilled nursing, therapy, or support managing a chronic condition, RubyWell can help us unlock the full potential of Medicare’s home health benefit and get help at home, faster and easier.
Medicare Home Health Care FAQs
How much does Medicare pay for home health care per hour?
Medicare doesn't pay the patient for home health care on an hourly basis. It reimburses home health agencies that provide the care. And that reimbursement rate differs depending on which kind of care professional is providing the care (skilled nurse, physical therapist, occupational therapist, speech therapist, home health aide). But the net take away for patients is that Medicare covers all medically necessary home health costs for eligible beneficiaries. So you will likely spend no money out of pocket if you’re eligible for home health care. If you’re covered by a Medicare Advantage plan, you may have to pay a co-pay for home health services.
How long will Medicare cover home health services?
Medicare covers medically-necessary home health care as long as it maintains the patient’s condition or slows their decline. This could continue for months or years.
How many hours of home health care does Medicare cover?
Medicare covers up to 28 hours of medically-necessary home health care per week, and that includes all care provided by a skilled nurse, physical, occupational, and speech therapists, and home health aide under the supervision of a skilled nurse in a given week. In certain medically-necessary cases, this limit can be extended to 35 hours per week. However, it’s rare that Medicare approves 35 or even 28 hours of home health care per week for a patient. Patients are approved for the number of hours required by their health condition and care needs. And no more than 8 hours of home health care can be provided per day.









