
- Home care is non-medical care that can provide help with activities of daily living, companionship, meal prep, errands, transportation, and light housekeeping.
- Home health care is skilled medical care that’s necessary to treat acute illness or injury, manage new diagnoses and difficult-to-manage chronic conditions, with the goal of preventing unnecessary hospital visits and reducing unnecessary costs.
- Hospice care is for people who have a terminal diagnosis and have a life expectancy of six months or less if the disease process runs its normal course; and who choose to have palliative (comfort) care instead of curative care.
- Medicare covers home health care and hospice care for eligible and qualifying beneficiaries.
When someone we love starts needing help to live safely at home, we can feel like we’re wandering through a maze of care options. Many of us want to be able to keep our loved ones in their homes (or ours) for as long as possible. So arrangements and benefits like home care, home health, and all hospice sound appealing. But those choices mean very different things for our family, our finances, and our loved one’s day-to-day life. Here, I’ll break down each of them, sharing what kinds of care each option provides, who they’re for, and what they can cost us.
Why understanding care options matters
Family caregiving can be very rewarding. But it can also be hard on our bodies, minds, and wallets. Many caregivers report worsening health, higher rates of depression, and thousands of dollars in out-of-pocket costs each year. And hospitalizations, emergency department (ED) visits and multiple doctor visits for aging adults are extremely expensive, for families and the health system.
Choosing the right type of in-home care can ease the intensity of family caregiving and protect our loved ones from avoidable trips to the hospital. And the good news: Medicare covers some types of in-home care for eligible beneficiaries. Since the relatives we care for have likely been paying into Medicare all of their working lives, it makes sense to take advantage of any covered care they may be entitled to. In some cases, Medicaid may also cover this care. So if the person we care for qualifies for Medicaid, we shouldn’t miss out on these benefits.
Home care vs. home health vs. hospice: Key differences
This chart is useful to compare the three kinds of in-home care.
Home care: Help with day-to-day living
Home care (often called “non-medical home care” or “personal care” or my least favorite: “unskilled care”) focuses on help with activities of daily living (ADLs). These include:
- Bathing/showering
- Personal hygiene (washing, grooming, oral care)
- Dressing
- Toileting
- Eating/feeding
- Transferring or mobility
- Continence
Home care can also provide companionship, meal prep, help with errands, transportation, and light housekeeping. Services are provided by caregivers or personal care aides.
Home care does not include skilled medical support from nurses or therapists in most instances.
Who can receive home care services?
Home care can be a good fit if our loved one:
- Is mostly medically stable but needs help with the ADLs and other daily tasks noted above
- Should not be left alone for long periods and benefits from companionship or supervision
- Lives with family caregivers who need respite to work, rest, or care for their own health
How to pay for home care
Because home care is not medical care, Medicare does not cover it. So how do we pay for it? We have a few options:
- Many long-term care insurance policies cover home care, and some will even pay a family member to provide this care.
- Most states have Medicaid waiver programs that cover home care services for people who meet Medicaid’s strict income and asset limits. And some states pay a family member to provide this care under specific programs like Consumer Directed Care Services (CDS).
- Some VA programs cover home care for eligible Veterans, and some programs pay a family member to provide care.
- Without any additional funding sources, the rest of us are left to pay for home care services out of pocket.
Home care can be provided on an hourly, around the clock, or live-in basis. We can access care through home health agencies or through individual caregivers. Not surprisingly, the hourly cost is about double when we go through an agency. But an agency will provide back-up caregivers as needed and handle all of the payroll, taxes, background checks, insurance bonding, some care plan oversight and more that can be incredibly valuable. When choosing an agency, we need to ask what kind of screening and ongoing oversight they provide for their caregivers.
Home health: skilled medical care
Home health care is skilled medical care provided in a patient’s home at the recommendation of an authorized provider like a doctor or nurse practitioner. Its goals are to treat illness or injury, return the patient to maximum level of rehabilitation, manage chronic conditions, prevent and slow further decline, and prevent hospital and ED visits.
Home health services include:
- Skilled nursing care such as wound care, medication management, injections, IV therapy, and health monitoring
- Physical, occupational, and speech therapy to improve strength, balance, daily function, communication, or swallowing
- Medical social work which can include patient and caregiver counseling, education, and referrals to resources
- Home health aide assistance with daily tasks when tied to the skilled care plan
Who can receive home health services?
Home health services have to be ordered by a patient’s doctor or qualifying nurse practitioner, a discharging hospitalist, or skilled nursing facility medical director or qualifying provider. In order for our loved one to get a home health referral order, a patient has to meet specific eligibility criteria, including:
- They must be homebound, which means it’s difficult, unsafe, or impossible for them to leave home without assistance from another person or a cane, walker, crutches, or wheelchair.
- They must have a health condition(s) and skilled care needs that increase their risk for hospitalization
- Due to their health condition(s), they need intermittent skilled care (see previous list)
Home health is common after a hospital stay, surgery, fall, or major change in health. It can also be ordered for people with chronic illnesses like heart failure, COPD, Parkinson’s disease or diabetes who are at risk for future hospitalizations.
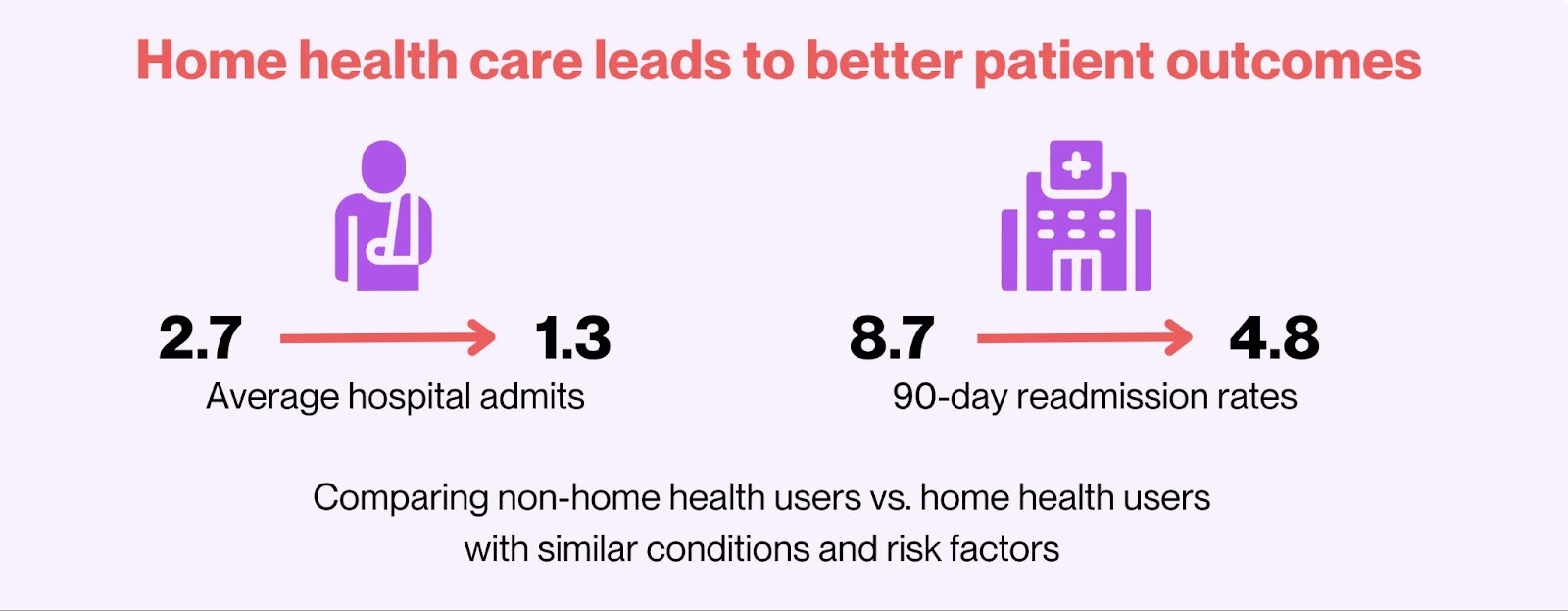
Medicare data show that older adults who receive medically necessary home health care tend to have fewer hospital readmissions and ED visits than patients with similar risk factors who don’t receive home health services.
How to pay for home health
Here’s the great news: Medicare, Medicaid, and most private health insurers cover home health for eligible beneficiaries.
The number and length of visits vary depending on the patient’s health condition and care needs. If our family member qualifies for home health services, their doctor or nurse practitioner will include a plan of care with the home health referral order. And the home health agency they’re referred to will develop a visit schedule that aligns with that plan of care.
The process of accessing home health care is pretty easy if our loved one is being discharged from a hospital or skilled nursing facility. The discharge manager gathers the referral order and sends it to a home health agency. The agency calls us and schedules the first visit within 48 hours in most cases. Done and done.
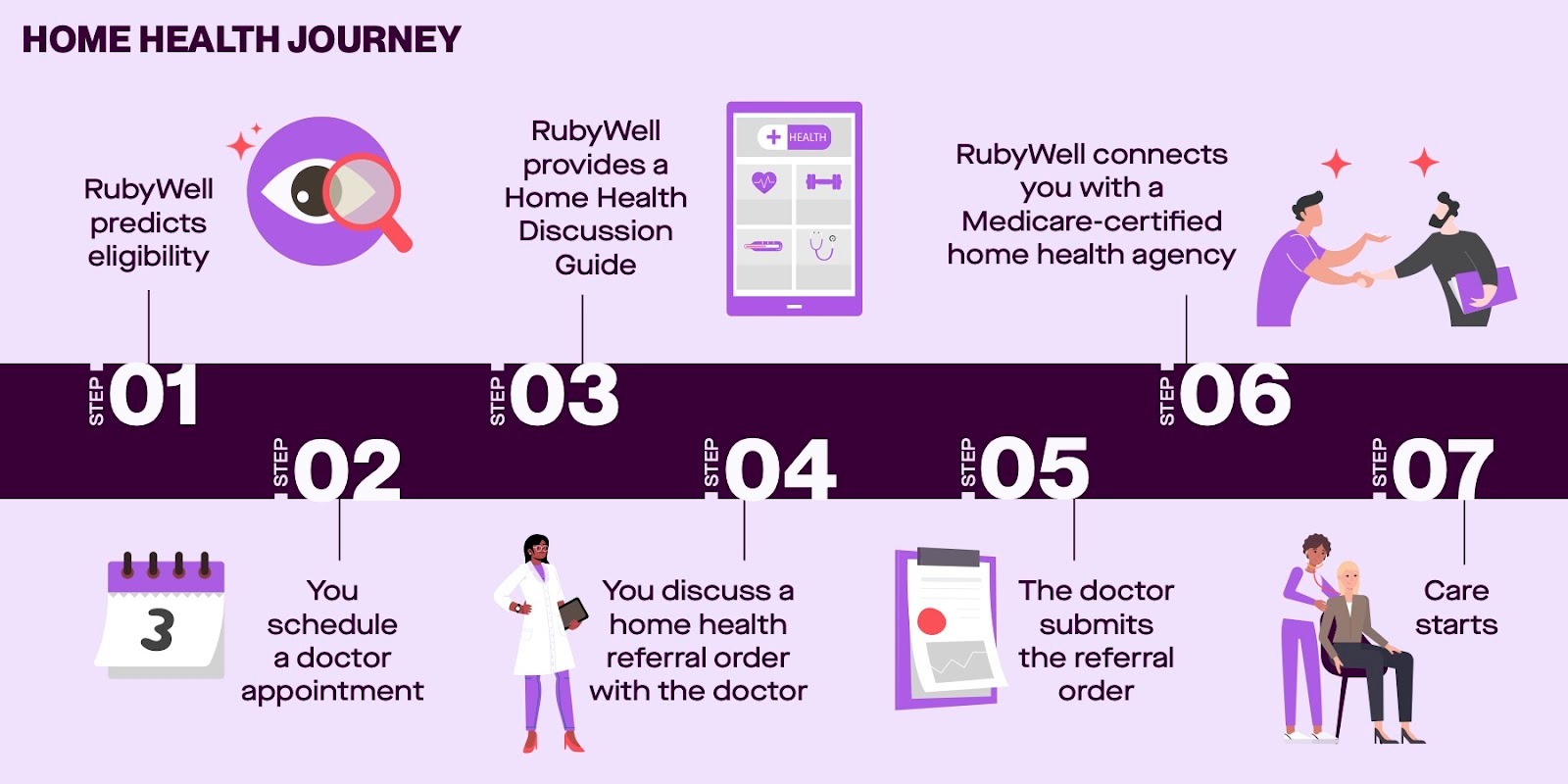
If we’re caring for someone who’s homebound and on Medicare, and hope to start home health services covered by Medicare, we have a few hoops to jump through.
- First, we need to find out if our loved one is even eligible for the benefit.
- If they are, we need to schedule an in-person or telehealth visit with their doctor or nurse practitioner to discuss the need for home health. During the appointment, we need to discuss the reason(s) that home health skilled services are being ordered. This appointment has to happen either 90 days before or within 30 days after Home Health Services start.
- If the doctor/nurse practitioner agrees that home health would be appropriate, they have to write a home health order that complies with Medicare regulations. This includes certifying that our loved one is eligible for services and providing care plan oversight.
- They then submit that order along with relevant medical information to a home health agency as a referral for care.
- The agency reviews the referral order, contacts the family caregiver or patient, and schedules the first visit within 48 hours in most cases.
There are a bunch of things that can slow this process down. For many patients, it can take weeks to get a doctor’s appointment. Some healthcare providers aren’t familiar with the home health benefit as it pertains to patients with chronic diseases, so they may think you’re not eligible, even if you are. Or, they may not know what to include in a compliant home health referral order. So the agency may have to follow up with the doctor’s office multiple times until the referral order is complete and compliant.
How RubyWell helps families unlock covered home health care
RubyWellTM has developed technology that predicts eligibility for the Medicare home health benefit, then provides the patient with a personalized Home Health Discussion Guide that they can take to their doctor’s appointment. The Discussion Guide lays out all of the patient’s health information that indicates that home health would be appropriate. And it gives the doctor or nurse practitioner the information they need to write a compliant home health order, the first time. It also includes the name and contact info for the partner home health agency the patient will be referred to. It really streamlines the process for all involved so care can start sooner.
For older adults, this can mean staying safely at home with skilled support instead of frequent hospital stays. For family caregivers, it means sharing the workload with professionals, protecting our own health, and easing financial pressure. It all starts with checking eligibility.
Hospice: Comfort-focused care at the end of life
The focus of Hospice care shifts from trying to cure illness to relieving suffering, supporting the family, and protecting quality of life as our loved one’s life draws to a close. Hospice can be provided wherever the person lives—at home, an assisted living facility, in a nursing home. Or it can be provided at a hospice facility. During the admission process, the hospice provider will talk with us to understand our family’s goals and where our loved one wants to receive care.
Hospice care typically includes:
- Nurses who manage pain, shortness of breath, nausea, anxiety, and other symptoms
- Home health aides to help with bathing, dressing, personal care, and light housekeeping tasks which can include meal preparation.
- Medications, equipment, and supplies related to the terminal diagnosis (like hospital beds, oxygen, and certain medications)
- Social workers, chaplains, and bereavement support for patients and families
- Other services like Music, Pet or Massage Therapy may also be available.
Each hospice may offer slightly different services, so it’s good to ask them what’s available.
Who can receive hospice care?
Hospice care is for people with a certified terminal illness who have a life expectancy of six months or less if the illness runs its usual course. The patient or their decision-maker needs to choose comfort care over curative treatment in order for the patient to be eligible for the benefit.
To arrange hospice care, we start by calling our loved one’s primary care doctor, specialist, hospital team, or a hospice agency directly to ask for a hospice evaluation. The doctor or hospice will review the medical history, recent hospitalizations and diagnoses, functional decline, and symptoms to see if hospice criteria are met. If they feel that all of the requirements are being fulfilled, they’ll place a referral order. If our loved one doesn’t have an attending physician, a hospice physician can perform the evaluation, make the determination, and certify that the person we care for meets the qualifications of terminal illness.
Many families say they wish they had started hospice earlier because of the suffering it alleviates for their loved one and the emotional and practical support it brings to them. I include myself with these families.
How to pay for hospice care
Medicare, Medicaid, and many private insurers cover hospice care for eligible patients at no cost for the services. If we decide on our own that our loved one needs to see another physician without the approval of the hospice provider, the hospice benefit will not cover that outside care.
Choosing the right next step
To find our way to the appropriate care, we need to start by asking ourselves: Is our loved one’s main issue an inability to perform daily tasks, medical needs, or end-of-life comfort?
If the main issue is “medical needs” and the person we care for is unable to leave home without help or special equipment, it makes sense to explore home health eligibility first, since it can be covered by Medicare. RubyWell can predict if our family member is likely to qualify and guide us through the gauntlet of accessing care.
From there, we may want to supplement the home health care with home care services for non-medical care. This could give us the respite we need to maintain our own health and continue to provide our best care. As our loved one nears the end of their life, their condition may decline to the point that we may need to call on hospice care to provide comfort care help to support them and us through that transition with dignity.
None of these care options is necessarily a final decision, and can evolve as our family’s needs change. What is important is what’s right for our family’s physical, emotional, and financial needs. And what’s right today may not be right in the future. Understanding all of the care options available will help us make choices that best support the health of the person we’re caring for as well as our own.









