
- Patients on Medicare Advantage (MA) plans often receive fewer home health visits and may experience worse outcomes compared with those on Original Medicare.
- MA Enrollees can switch to Original Medicare or a different MA plan during the MA Open Enrollment Period (OEP): Jan 1-Mar 31, or the MA Annual Enrollment Period (AEP): Oct 15-Dec 7.
- Every state has a State Health Insurance Assistance Program (SHIP) that offers free, one‑on‑one Medicare counseling to older adults, their families, and caregivers.
- RubyWell can help predict if a Medicare patient may qualify for the Medicare home health benefit, and guide them through the process of accessing care.
Marjorie’s 83-year-old father, Harold, had been pretty happy with the coverage provided by his Medicare Advantage (MA) plan. While the provider network was a little restrictive, it included his favorite doctors. He also liked that the plan included prescription, vision, and dental coverage, all for one manageable monthly premium.
But when Harold was discharged from the hospital after a health event caused by a worsening chronic condition, Marjorie learned that his MA plan would only authorize a handful of home health visits. After the visits were completed, Harold’s condition didn’t allow for him to care for himself without additional assistance. So it was up to Marjorie to manage medical tasks that she had received little to no training for.
How does Medicare Advantage cover home health care?
All MA plans have to cover home health services using the same criteria as Original Medicare. Home health services include:
- Skilled nursing
- Physical therapy
- Occupational therapy
- Speech therapy
- Home health aide services under the supervision of a skilled nurse
- Medical social work
However, many MA enrollees are surprised to learn how few home health visits their plan allows, at the very time they need the care most. Coverage provided by Original Medicare (Parts A and B) is not limited as long as the patient continues to meet coverage requirements. So, why is there a difference in the amount of home health MA plans cover?
When MA plans don't cover the care, or only cover a few visits, it may be because the MA plan is making a “utilization management” decision. They’re deciding that the care is not medically necessary. Unfortunately, this decision can force home health agencies to discharge some patients prematurely. And that can result in poor health outcomes, avoidable re-hospitalizations, and unprepared, burned‑out family caregivers.
Beneficiaries like Harold do have rights in this situation. He and his daughter could have appealed the MA plan's decision. And if the plan didn’t approve more care upon appeal, Harold would have been entitled to an independent review by an unbiased third party. But that’s a lot of hoops to jump through. Especially for a homebound older adult and a busy, stressed out family caregiver who’s trying to manage all of the home health tasks on her own.
Another challenge with accessing home health care through a Medicare Advantage plan is that some of the plans pay home health agencies less than it costs the agencies to provide the service. As a result, agencies don’t accept patients on those plans. If the person we care for doesn’t live near a home health agency that accepts their plan, how do they access the covered care they're entitled to?
As our loved ones age and begin to lose their ability to care for themselves, it’s important that we, as family caregivers, get a clear understanding of their home health coverage. Primarily, it will fall to the family to pick up the slack and make ongoing care decisions.
The good news is, if a loved one’s MA plan’s home health coverage is disappointing, they have two different opportunities during the year to switch to Original Medicare or a different MA plan:
- Medicare Advantage Open Enrollment: January 1 - March 31
- Medicare Advantage Annual Enrollment: October 15 - December 7.
More about this in a bit.
Why home health coverage matters
Home health is medical care provided by skilled nurses, physical, occupational, and speech therapists, and home health aides under the direction of a certifying provider (e.g. a doctor or nurse practitioner). Care provided can include medical support like wound care, medication management, ostomy and catheter care, health management and monitoring, as well as therapies that help improve strength and mobility so that a patient may safely move about the house, swallow food safely, perform activities of daily living, and more.
Home health is often ordered by a hospital when an older adult is discharged after an inpatient stay. A primary care physician or other certifying medical provider can also order home health for a patient who’s living in the community as long as they meet both of these criteria:
- They can’t leave home without assistance from another person or a medical device such as a cane, crutches, walker or wheelchair.
- They have health conditions and care needs that increase their risk for hospitalization.
The certifying provider must provide a signed, certified home health order before home health services can begin.
Home health is often the difference between living safely at home and a revolving door of ER visits and hospital readmissions. For frail, homebound patients, losing skilled support too early increases risk of falls, infections, medication errors, uncontrolled chronic conditions and complications that land them back in the hospital.
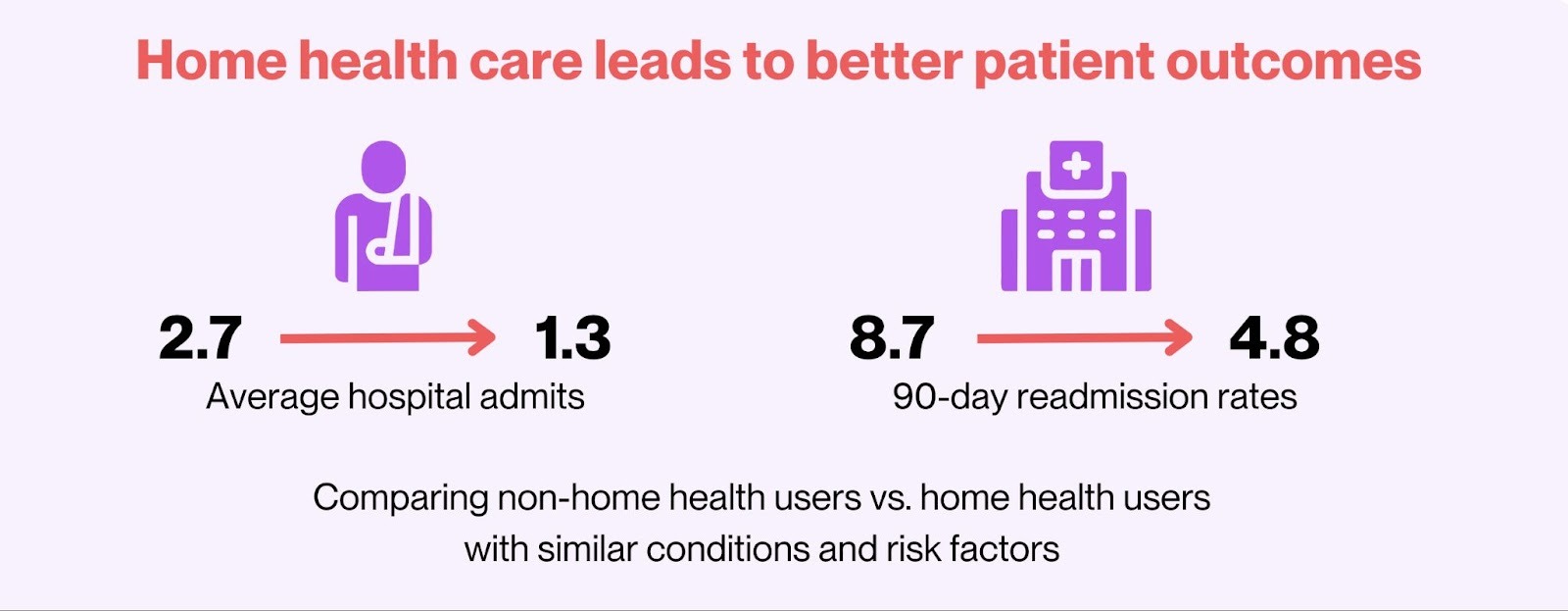
Source: Evaluation of Home Health Expenditures in a Medicare-Eligible Population
Medicare Advantage vs. Original Medicare
Original Medicare (Part A and Part B) covers home health services for eligible, homebound beneficiaries for as long as care remains medically necessary and they meet all eligibility criteria. Full stop.
MA plans, which are offered and managed by insurance companies, must cover at least the same home health benefits as Original Medicare, But MA plans can manage that benefit very differently. Many MA plans require prior authorizations, visit caps, narrow networks, and copays, all of which could translate into fewer visits and earlier discharge from home health.
Research has shown that patients on MA often receive fewer home health visits and may experience worse outcomes compared with those on Original Medicare, including more adverse health events, care disruptions, and less functional improvement. And who absorbs the fallout? Family caregivers. We may find ourselves having to do complex wound care, injections, or rehab support that we haven’t been trained to do. That can lead to stress, burnout, and sometimes our own health crises. And no one really wins, because these strains can cause patients to wind up back to the ER as a “last resort,” raising overall costs for Medicare.
RELATED READING: Original Medicare vs. Medicare Advantage: Key Differences for Family Caregivers
Signs our loved one’s MA plan isn’t enough
There are a few red flags we can look for. Let’s look at Marjorie's and Harold’s situation.
🚩Harold’s home health visits were cut back even though he was still weak and unable to get from his bed to the bathroom without assistance. And they were cut off entirely while he was still unsafe walking and struggling with self‑care.
🚩Harold’s skilled nurse told Marjorie that she thought more care would be helpful. But when Marjorie asked the home health agency for more services, they told her that Harold’s MA plan would not approve more visits.Majorie might have been able to appeal this discharge decision but was never provided with guidance or expertise to even successfully attempt the appeal process. The paperwork she received was overwhelming and left her feeling like an appeal wouldn’t be successful even if she tried.
🚩After Harold’s home health services ended, Marjorie found herself struggling to provide the medical care that her father still needed—care tasks she had received no formal training for— leaving her feel unsure, afraid, at times and alone.
If any of these red flags sound familiar, it doesn’t mean home health “isn’t covered by Medicare.” It may mean our loved one’s MA plan is limiting services in a way that would look very different under Original Medicare.
Two opportunities to switch Medicare coverage
Luckily, the person we care for doesn’t have to stay on their MA plan. There are two windows when they can make a switch.
Medicare Advantage Open Enrollment: January 1 - March 31
There’s a special window every year for current Medicare Advantage members who want to change their coverage. It’s called the Medicare Advantage Open Enrollment Period (OEP).
From January 1 through March 31, if the person we care for is on an MA plan, they can make one of two changes:
- Switch to a different MA plan that may offer better coverage
- Switch to Original Medicare
It’s smart to review our loved one’s current coverage and explore new options before the OEP deadline. If we do decide to make a change, the new coverage will go into effect on the first day of the following month. So if they switch plans on February 10, the new coverage begins March 1—this is important to keep in mind if we’re planning home health services and follow‑up appointments.
If we think it’s best for our loved one to switch back to Original Medicare during the OEP, they can also add a Part D plan and a Medigap plan at that time.
Note: When switching from MA back to Original Medicare, the Medigap plan providers can underwrite the Medigap policy. This means they can increase the Medigap premium, or even deny coverage, if our loved one has pre-existing conditions. So this could increase costs and limit Medigap plan options.
Medicare Advantage Annual Enrollment: October 15 - December 7
There’s also the Medicare Annual Enrollment Period (AEP), which runs from October 15 through December 7 every year. Anyone with Original Medicare or a Medicare Advantage plan may choose to keep or change their coverage at this time. Changes made during the AEP go into effect on January 1 of the following year.
Key considerations:
- Prescription drugs are not covered under Original Medicare, so if switching from MA to Original Medicare, the person we care for should consider purchasing a Prescription Drug Plan (Part D), as well.
- If they want to purchase a Medicare Supplemental Insurance (MediGap) plan that can cover some health expenses that Original Medicare doesn’t cover, they will have to go through the underwriting process. This will take into account pre-existing conditions which could make a MediGap plan more expensive.
- If they want to choose a different MA plan that offers better home health coverage, check to see if their favorite doctors and care facilities are in the new MA plan’s network. And ask their home health agency if they work with that MA plan. Just because an agency is in a plan’s network doesn’t mean they will work with that plan.
How SHIP can help your family
This is a lot to think about. But we don’t have to figure this out alone. Every state has a State Health Insurance Assistance Program (SHIP) that offers free, one‑on‑one Medicare counseling to older adults, their families, and caregivers. SHIP counselors are trained, unbiased, and do not sell insurance. So we don’t have to worry about any conflicts of interest.
A SHIP counselor can:
- Explain the differences between our loved one’s current MA plan and Original Medicare, including how each handles home health care and networks.
- Help us compare plans in our area, check drug coverage, and understand costs before our loved one makes a change.
- Walk us through the steps to switch plans during either enrollment period, if that’s the right choice for our loved one.
We can find our local SHIP at shiphelp.org.
Where RubyWell fits in
RubyWellTM is a technology company focused on helping families and care providers manage health safely at home. RubyWell’s tools can help predict if a Medicare patient may qualify for the Medicare home health benefit, based on their health condition and homebound status.
When someone appears likely to qualify, RubyWell guides the patient and family through the next steps—how to talk with the doctor, how to get a referral order, and how to connect with a trusted partner home health agency. That kind of support can reduce delays, help our loved ones get the services they’re eligible for, and ease caregiving intensity for family caregivers.
Currently, RubyWell works with patients who have Original Medicare or certain MA plans.
Steps we can take now
If we’re worried that our loved one’s Medicare Advantage plan isn’t covering enough home health support, but we’re not in an open enrollment period, we can:
- Call our loved one’s home health agency or doctor and ask directly whether more home health visits are medically necessary and whether coverage is being limited by the plan.
- Contact our state’s SHIP for free help reviewing options before either of the enrollment periods, so we can plan ahead for future coverage changes and make them quickly.
- Explore tools like RubyWell that can predict eligibility for home health services. Through the RubyWell process, we will learn if our loved one’s MA plan is one that they work with.
Family caregivers aren’t “being difficult” by asking questions about coverage. We’re protecting our loved ones—and ourselves—from avoidable crises. And we’re making sure Medicare works the way it’s meant to.









